Cancer itself is a serious challenge for the patient and his or her relatives. But in addition to the high risks of cancer itself, there are many co-morbidities associated with cancer. To protect your own or your loved one’s health, we suggest you familiarize yourself with the aspects and risks of cancer nutrition.
First of all, I would like to focus on the factors that determine our health:
- Contribution of health care – 10%
- Genetics and ecology – 40%
- Lifestyle and nutrition – 50%
Lifestyle and nutrition is a big modified factor and depends entirely on us. It depends on how properly and varied we eat, how our lifestyle is formed, whether there are bad habits – smoking and alcohol. How effectively we fight stress, work and rest regimes are important, and of course the level of physical activity.

For normal life support, the body must receive 76 nutrients (chemical elements necessary for living organisms to function normally), and 45 of them are usually essential.
Irreplaceable are those components in the diet that the body cannot synthesize on its own and must be obtained from the outside. They include most vitamins, micronutrients, omega-6, omega-3 fatty acids. And how proper your diet is, it is either a prevention or a risk factor for disease development, and cancer is no exception.
Most cases of cancer result in malnutrition. One in two cancer patients shows signs of malnutrition, and between 38% and 78% of cases actually have emaciation.
Many patients think that with optimal nutrition they are feeding not only themselves but also their tumor. But, this is not entirely true. It is proper nutrition that contributes to good tolerance of quite aggressive anti-tumor treatment and improves the patient’s well-being. Conversely, insufficient nutrition lowers immunity, which contributes to the progression of the tumor process, and, of course, reduces the quality of life of patients.
Causes of malnutrition can be anorexia or lack of appetite. Much depends on the location of the tumor, which sometimes simply does not allow for proper nutrition. Weight problems can also occur due to various complications of anti-tumor treatment, manifested by nausea, vomiting, and varying degrees of mucositis.
All of this, of course, can lead to metabolic changes and so-called “cancer cachexia”.
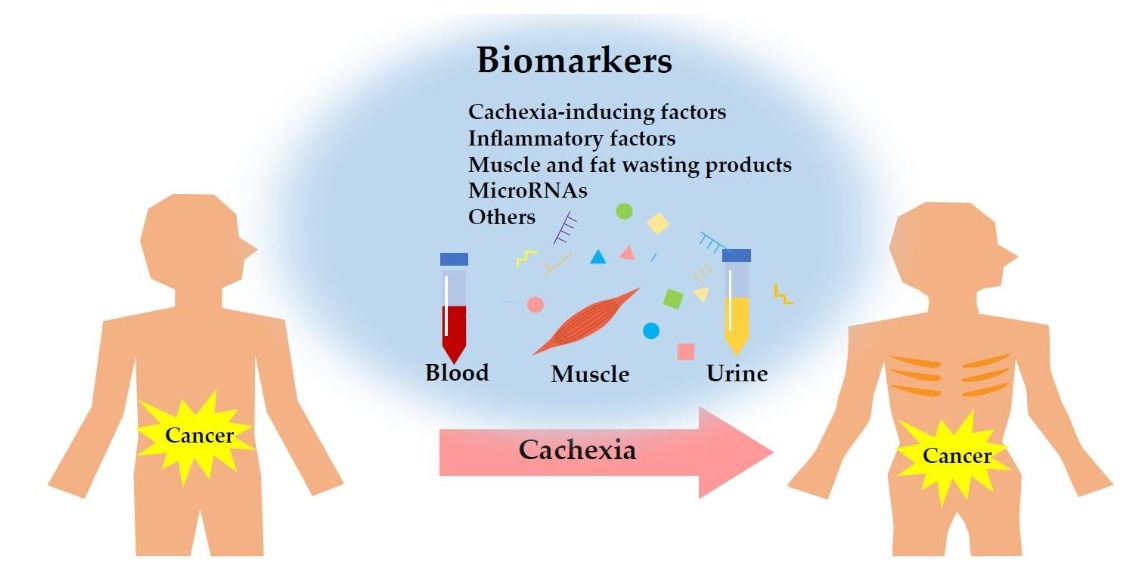
Cancer cachexia is a complex multifactorial metabolic syndrome during which decreased appetite, digestive distress, pain, depression, and changes in metabolism provoke the exhaustion of muscle mass in the body and the body in general.
This is caused by a chronic inflammatory process that is constantly supported by various cytokines, such as IL-1, ID-6, tumor necrosis factor alpha, and cachectin, which leads to decreased appetite and exacerbates malnutrition.
Cancer cells use host tissue for their growth and proliferation, which is why it is so important for the body to have adequate nutrition to make up for all the losses that occur in such a complex pathological process.
Stages of cachexia
- Pre-cachexia. It is diagnosed when no more than 5% of body weight is lost in six months. Against this background, there is a pathological aversion to food, as well as signs of inflammation: temperature over 38°C or below 36°C, rapid breathing, increased pulse rate to 90 beats per minute or higher.
- Cachexia. When a patient loses more than 5% of his body weight, he is diagnosed with the cachexia stage. It is accompanied by the same signs as those observed in pre-cachexia.
- Refractory cachexia. Develops with further progression of the pathological condition. The patient no longer responds to the prescribed treatment, so the measures taken to gain weight do not help either.
It is very important to diagnose cachexia in time and start treatment measures at the pre-cachexia, cachexia phase, because at the refractory cachexia stage treatment is almost useless and leads to death.
IMPORTANT
- Cachexia is diagnosed in 50-80% of cancer patients.
- With cachexia, treatment efficacy and treatment tolerance worsen.
- In over 20% of cases, cachexia is the cause of death from cancer.
Sarcopenia also often accompanies cachexia, whereas cachexia can be seen by the patient’s appearance, sarcopenia is difficult to see with the naked eye and requires good diagnosis.
The term “sarcopenia” has been around since 1988, and in Greek it means muscle deficiency.
DIAGNOSTIC TECHNIQUES FOR SARCOPENIA
·The simplest method of diagnosis is anthropometric data and caliperometry data (shoulder muscle circumference).
·The most accurate examinations are such as densitometry, bioimpedanceometry (body composition). This determines the amount of fat and muscle tissue.
And it is especially important to do such a study over time in order to keep track of which component is responsible for weight loss.
·Computed tomography can also help identify sarcopenia, which uses a skeletal-muscular index. The amount of muscle tissue – this index should be used when prescribing and choosing the dosage of chemotherapy. Because in this case, this individualized calculation allows the patient to tolerate chemotherapy and radiation therapy more easily, and fewer side effects are monitored.
SARCOPENIA AND SURVIVAL RATE
It is well known that sarcopenic obesity reduces life expectancy by 10 months. And, unfortunately, sarcopenic obesity is not uncommon nowadays, so it is very important to pay attention, diagnose and not to miss sarcopenia when the patient is overweight, when there is a lot of fat tissue and very little muscle tissue.
Back in 2011, there was a study that showed that enough skeletal-muscular mass makes it possible to tolerate radiation and chemotherapy well.
With this in mind, timely screening, diagnosis, identification of nutritional deficiencies, formation of nutritional support, and monitoring are very important.
There are several scales in the international community for diagnosing, screening for malnutrition.
The first scale proposed in 2002 by the European Society for Clinical Nutrition and Metabolism-Nutritional Risk Screening, the test consists of four questions:.
- What is your body mass index (should be at least 20.5)?
- Has there been a decrease in nutrition in the last week?
- Has your body weight decreased in the last 3 months and by how much?
- The presence of a serious illness?
If the answer is “no” to all four questions, the test is repeated one week later. If at least one answer is positive, a further, more in-depth examination takes place. All of this is necessary in order to choose the most adequate nutritional option.
The second screening scale is a subjective assessment. Here, not only anthropometric data, but also physical parameters of the body are taken into account.
The Nutritional Risk Index is the third screening scale. It is a formulaic calculation that takes into account body weight and serum albumin levels.
While the first screening scale is used for hospitalized patients, the third index is particularly effective for gastrointestinal cancers.
NUTRITIONAL SUPPORT. STAGES OF IMPLEMENTATION
- The first step is the calculation of needs.
- Next, energy deficiency and protein deficiency are diagnosed.
- Determination of the way of introducing nutritional support.
- Development of a nutritional strategy.
TYPES OF CLINICAL NUTRITION
Sipping is the consumption of a ready-mixed meal with a tube in small sips. This type of feeding is used for patients for whom regular nutrition does not meet all the body’s needs. It is convenient because it is already balanced and portioned. It can be used both in a hospital, outpatient clinic, and at home.
Probe feeding – when food is administered directly into the stomach or intra-intestinally with a probe.
This nutrition is used when the gastrointestinal tract is functioning but the patient is not able to receive nutrition on his or her own in the usual way. This can be caused by stenosis of the esophagus by a tumor, an early postoperative period, or being in the intensive care unit. If there is no possibility to use a probe, a stoma is put on and the same mixtures are used as for probe feeding.
Parenteral nutrition is auxiliary and should preferably be used in its pure form, acceptable only for a limited period of time. Because the main parameter is that it is necessary to use as much as possible the gastrointestinal tract if it works and to start its work if there are difficulties. Because interoral nutrition is more physiological and causes fewer complications, it is the prevention of atrophy of the intestinal villi and it is cheaper than peripheral nutrition.
There is a fairly wide range of specialized clinical nutrition. These are various “nutricks” with many flavors, it is a probe nutrition semi-elemental, which is used for intestinal insufficiency, malabsorption syndrome, short bowel syndrome inflammatory intestinal diseases.
There are also immune mixtures, which are also quite promising and interesting, specialized mixtures specifically for patients with diabetes, who have damage and diseases of the kidneys, liver.
For cancer patients will be especially relevant hypo-energetic mixtures with high protein content, which in a small amount contain a large number of calories and various nutrients: vitamins, trace elements.
I would like to emphasize that the quality of life of a cancer patient depends 30% on the location of the tumor, 20% on nutrition, 30% on weight loss, and the rest of the parameters are much less.
Therefore, it is worth reminding you that it is not only important for a cancer patient to have an oncologist, but also to have the advice of a qualified nutritionist. A proper, balanced diet can not only make your cancer treatment easier, but also help you avoid cancer.