Do you know that a single 30-minute procedure can identify tissue changes years before they become cancerous? During colonoscopy, gastroenterologists and colorectal surgeons examine the entire large intestine using a flexible tube equipped with a high-definition camera, identifying small changes that could develop into cancer if left untreated.
Modern colonoscopy equipment provides wide viewing angles and high magnification, allowing specialists to distinguish between benign tissue variations and potentially dangerous lesions. The procedure’s dual capability, simultaneous detection and removal of polyps, sets it apart from other screening methods. While CT colonography and stool DNA tests can indicate abnormalities, only colonoscopy enables immediate tissue sampling and polyp removal during the same session.
Singapore’s colonoscopy screening guidelines recommend beginning at age 50 for individuals without risk factors, with procedures repeated every 10 years if results remain normal. A colonoscopy doctor Singapore may advise earlier screening for those with family history of colorectal cancer or inflammatory bowel disease, typically starting 10 years before the age their relative was diagnosed, or at age 40, whichever comes earlier.
Visual Detection Techniques During Colonoscopy
White Light Examination
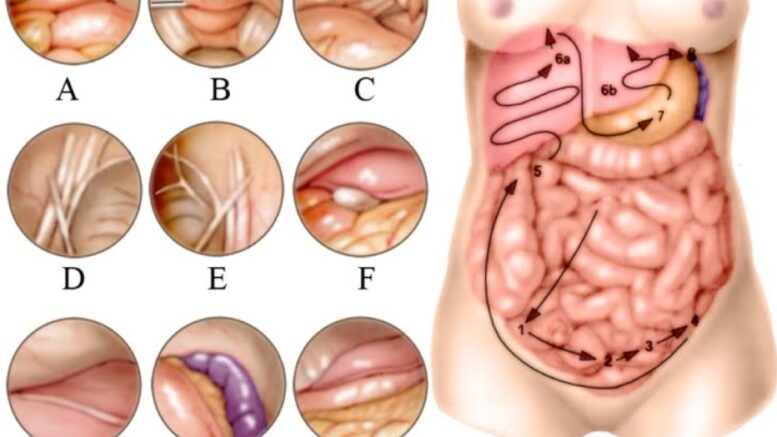
Standard white light colonoscopy illuminates the colon’s surface to reveal color variations, surface patterns, and structural abnormalities. Polyps appear as raised lesions protruding from the intestinal wall, ranging from flat patches barely 2mm high to pedunculated growths on stalks extending 20mm or more into the lumen. Colonoscopy practitioners recognize color differences, hyperplastic polyps often appear pale or match surrounding tissue, while adenomatous polyps display darker, reddish hues due to increased vascularity.
Surface texture provides additional diagnostic clues. Smooth, dome-shaped lesions suggest hyperplastic polyps, while irregular, lobulated surfaces indicate adenomas with higher malignant potential. Villous adenomas exhibit finger-like projections visible under standard lighting, signaling increased cancer risk requiring removal.
Chromoendoscopy and Dye-Spraying Methods
Chromoendoscopy involves spraying contrast dyes directly onto the colon lining during colonoscopy, highlighting surface patterns invisible under white light. Indigo carmine, a blue contrast agent, pools in mucosal crevices to outline polyp borders and reveal flat lesions that blend with normal tissue. This technique increases detection rates for flat adenomas compared to standard examination.
Methylene blue staining allows cellular-level visualization by being absorbed selectively by normal colonic cells while abnormal tissue remains unstained. This differential uptake creates a detailed map of suspicious areas, particularly useful for detecting dysplasia in patients with inflammatory bowel disease. The staining process adds 5-10 minutes to procedure time but improves identification of precancerous changes.
Narrow Band Imaging (NBI)
NBI technology filters white light into specific blue and green wavelengths that penetrate tissue at different depths. Blue light (415nm) highlights surface capillaries, while green light (540nm) reveals deeper blood vessels. This creates detailed vascular maps distinguishing benign from precancerous lesions without requiring dyes or prolonging procedures.
Adenomatous polyps display characteristic brown vessels surrounding white structures, the “brown blob” pattern, while hyperplastic polyps show uniform pale vessels. Cancerous lesions exhibit chaotic, irregular vascular patterns with abrupt vessel terminations. NBI classification systems achieve accuracy for differentiating polyp types, helping doctors decide which lesions require removal versus monitoring.
Types of Early Changes Detected
Adenomatous Polyps
Adenomatous polyps represent a common target of colonoscopy screening, as these lesions follow the adenoma-carcinoma sequence. Tubular adenomas display organized glandular structures with minimal cancer risk when smaller than 10mm. Tubulovillous adenomas contain mixed architecture with intermediate malignant potential, while villous adenomas carry higher cancer risk due to their finger-like projections and typically larger size.
Size directly correlates with cancer risk: smaller adenomas have negligible immediate risk, while larger polyps carry increased cancer probability. Location also influences risk assessment, right-sided polyps often grow flatter and broader, making detection more challenging, while left-sided lesions typically present as discrete, pedunculated growths.
Hyperplastic Polyps
Hyperplastic polyps appear most commonly in the rectum and sigmoid colon as pale, flat lesions under 5mm. These benign growths rarely progress to cancer, though large hyperplastic polyps in the right colon may harbor malignant potential through the serrated pathway. Microscopic examination reveals saw-toothed crypts without dysplasia, distinguishing them from sessile serrated adenomas that share similar appearance but carry cancer risk.
Sessile Serrated Lesions
Sessile serrated lesions (SSLs) challenge detection due to their flat morphology, indistinct borders, and color matching surrounding mucosa. These lesions preferentially develop in the right colon, often covered by mucus caps that obscure visualization. SSLs can lead to colorectal cancers through the serrated neoplasia pathway, developing more rapidly than conventional adenomas.
Recognition requires careful observation for subtle signs: interruption of normal vascular pattern, mucus adherence despite washing, and rim of debris surrounding the lesion. Larger size or presence of dysplasia mandates complete removal with clear margins, as these features indicate increased cancer risk.
Inflammatory Changes
Colonoscopy identifies inflammatory patterns suggesting conditions like ulcerative colitis or Crohn’s disease before symptoms develop. Early ulcerative colitis presents as granular mucosa with loss of vascular pattern, progressing to continuous inflammation from rectum proximally. Crohn’s disease displays patchy inflammation, linear ulcers, and cobblestone appearance from alternating inflamed and normal tissue.
Pseudopolyps, islands of normal tissue surrounded by ulceration, indicate previous severe inflammation. While benign themselves, their presence signals increased cancer risk requiring enhanced surveillance. Dysplasia-associated lesions or masses (DALMs) in inflammatory bowel disease patients appear as irregular, velvety patches requiring biopsy and potential colectomy if confirmed dysplastic.
Technology and Equipment
High-Definition Imaging Systems
Current colonoscopy systems employ high-definition cameras with 1.2 million pixels or greater, providing improved resolution compared to standard definition equipment. This enhanced clarity reveals surface patterns, color variations, and vascular networks that may not be visible with older technology. Digital processors analyze images in real-time, adjusting brightness and contrast to optimize visualization in different colon segments.
Wide-angle lenses expanding viewing fields to 170 degrees reduce blind spots behind folds and flexures where polyps commonly hide. Some systems incorporate dual cameras providing forward and retrograde views simultaneously, improving detection in difficult anatomical areas. Image enhancement features including electronic chromoendoscopy and surface pattern recognition assist in real-time polyp characterization.
AI-Assisted Detection Systems
Artificial intelligence algorithms trained on colonoscopy images now assist doctors in identifying suspicious lesions. These systems highlight potential polyps with visual markers. AI can detect flat lesions and sessile serrated polyps that human observers may miss.
Computer-aided detection (CADe) systems analyze video streams in real-time, alerting endoscopists to review areas containing possible abnormalities. Studies demonstrate AI assistance can increase adenoma detection rates without significantly prolonging procedure time. Singapore facilities increasingly incorporate these technologies, though human expertise remains important for clinical decision-making and polyp removal.
Did You Know?
The colon’s natural folds create blind spots during forward telescope withdrawal. Retroflexion techniques and careful fold examination compensate for these anatomical challenges.
Quality Indicators and Detection Rates
Adenoma Detection Rate (ADR)
ADR measures the percentage of screening colonoscopies where at least one adenomatous polyp is identified and removed. Quality benchmarks set minimum ADRs at 30% for male patients and 20% for female patients. Each 1% increase in ADR correlates with 3% reduction in interval cancer risk, emphasizing this metric’s clinical importance.
Factors influencing ADR include:
- Withdrawal time
- Bowel preparation quality
- Endoscopist experience
Withdrawal requires minimum 6 minutes examining mucosa during scope removal, when most polyps are detected. Bowel preparation, achieving Boston Bowel Preparation Scale scores of 2-3 in each segment, ensures complete visualization. Endoscopists performing over 200 colonoscopies annually maintain higher detection rates through pattern recognition expertise.
Withdrawal Time and Inspection Technique
Systematic withdrawal technique maximizes polyp detection through deliberate mucosal inspection. Examination requires:
- Deflation to flatten folds
- Position changes to redistribute fluid
- Retroflexion in the rectum to visualize the anal canal
Cleaning residual stool and mucus with targeted water jets reveals hidden lesions.
Segmental inspection involves examining each anatomical section twice, during insertion and withdrawal, with particular attention to flexures where polyps concentrate. The hepatic flexure, splenic flexure, and rectosigmoid junction harbor disproportionate numbers of missed lesions due to sharp angulation. Careful navigation with controlled tip deflection and torque ensures complete visualization of these challenging areas.

What Our Colorectal Surgeon Says
Polyp detection requires both technological capability and clinical pattern recognition developed through experience. Modern colonoscopy combines multiple imaging modalities, white light, NBI, and sometimes chromoendoscopy, adapting technique to each patient’s anatomy and pathology.
The decision to remove versus monitor a polyp depends on multiple factors assessed during the procedure. Size, morphology, surface pattern, and location all influence management. Small hyperplastic polyps in the rectum require no intervention, while any adenomatous polyp warrants removal regardless of size.
The colon lacks pain receptors, making polypectomy painless. The electrical current used for removal cauterizes blood vessels simultaneously, minimizing bleeding risk. Large polyps may require piecemeal removal with subsequent surveillance to ensure complete excision.
Putting This Into Practice
- Schedule colonoscopy screening at the appropriate age if you have no risk factors, or earlier if family history exists
- Request your colonoscopy report include specific quality metrics like withdrawal time and bowel preparation score
- Ask about the technology available at your chosen facility, HD imaging and NBI improve detection rates
- Follow bowel preparation instructions carefully, as poor preparation obscures lesions
- Discuss surveillance intervals based on findings with your healthcare professional, normal results permit longer intervals, while polyp removal requires shorter follow-up
When to Seek Professional Help
- Blood in stool or on toilet paper
- Changes in bowel habits persisting beyond two weeks
- Unexplained abdominal pain or cramping
- Narrow, pencil-thin stools
- Feeling of incomplete evacuation after bowel movements
- Unexplained weight loss
- Chronic diarrhea or constipation
- Family history of colorectal cancer or polyps
- Previous polyp removal requiring surveillance
- Inflammatory bowel disease diagnosis
Commonly Asked Questions
How accurate is colonoscopy in detecting early cancer?
Colonoscopy identifies precancerous adenomas with high sensitivity for larger lesions. Smaller polyps may be missed in some examinations. These missed small lesions rarely contain cancer and typically require years to develop malignant potential.
What’s the difference between virtual colonoscopy and traditional colonoscopy?
Virtual colonoscopy (CT colonography) uses computed tomography to create 3D colon images without scope insertion. While less invasive, it cannot remove polyps, requires bowel preparation, and misses some flat lesions. Positive findings necessitate traditional colonoscopy for polyp removal. Radiation exposure and inability to sample tissue make virtual colonoscopy unsuitable for high-risk individuals.
Can colonoscopy miss polyps or cancer?
Colonoscopy may miss some small polyps and a smaller proportion of larger adenomas. Flat lesions, poor bowel preparation, and inadequate withdrawal time increase miss rates. Interval cancers developing between screenings can occur, often arising from missed or incompletely removed lesions.
How do doctors decide which polyps need immediate removal?
All adenomatous polyps require removal due to malignant potential. Hyperplastic polyps under 5mm in the rectosigmoid typically need no intervention. Larger polyps, those with atypical features, or any lesion in the right colon warrant removal for histological examination. Advanced imaging helps predict histology, but definitive diagnosis requires tissue analysis.
Next Steps
Colonoscopy prevents colorectal cancer by removing precancerous polyps before malignancy develops. Schedule screening at age 50, or earlier with family history. Request facilities offering high-definition imaging and narrow band imaging technology for optimal detection rates.
If you’re experiencing rectal bleeding, persistent changes in bowel habits, or unexplained abdominal pain, a MOH-accredited colorectal surgeon can provide comprehensive evaluation using modern detection technology.